

For decades, marijuana was known as an illegal drug and a subculture of its own, far from the mainstream. In recent years though, scientists have found more and more evidence of its therapeutic potential. Cannabis has become a trusted, daily medication for millions of people across the world, treating conditions ranging from anxiety to arthritis to the nausea caused by chemotherapy, without the dangerous and harmful side effects of many popular pharmaceuticals.
The world of cannabis also has an entire language all of its own. In this introduction to medical marijuana, we’ll break down how cannabis works, how patients can use cannabis, what to look for when deciding which cannabis product to use, and how to get a medical card in minutes.
In the early 1990s, researchers discovered a previously unknown communication system involved in the regulation of nearly every essential function in the body. They named it the endocannabinoid system (ECS) after the plant elements that led researchers to its discovery — cannabinoids.
This system is made up of cannabinoid receptors (called CB1 and CB2), endocannabinoids (natural chemicals in the human body which activate or modulate CB1 and CB2 activity), and enzymes which metabolize the endocannabinoids and clear them from the body.
With most medications, dosing is pretty simple — there are clinical trials, FDA approval, and recommendations handed down to doctors and pharmacists based on specific chemical calculations.
For cannabis, dosing is not yet an exact science and a much more individualized approach is required.
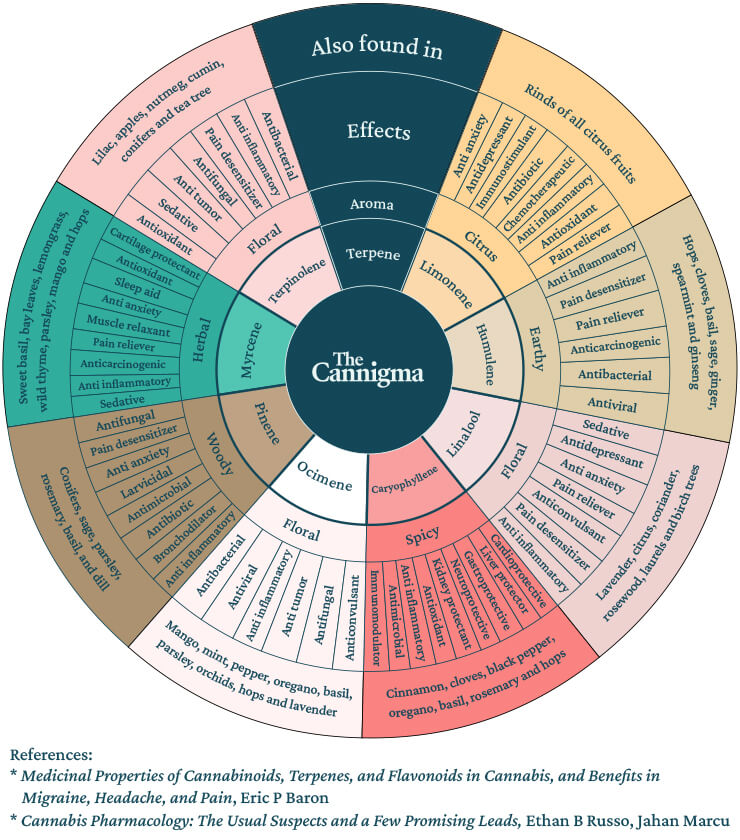
A doctor prescribing cannabis must consider the best delivery methods for their patient as well as the right CBD-to-THC ratio, terpenes, or which strain of marijuana is best for the patient.
Today’s marijuana products can be quite potent so patients should be advised to “start low and go slow,” by taking a low dose and then increasing it as needed, after gauging the effects. The first time using cannabis should also be done in a comfortable place and with a trusted confidant.
Cannabis is typically taken 2-3 times daily and most patients do not exceed 1–3 grams of cannabis per day. In general, patients tend to develop tolerance to the psychotropic effects of THC rather quickly, but this doesn’t result in a reduction in the therapeutic benefits.
In addition to how one takes cannabis, the type of cannabis is also very important. Cannabis “strains” are often divided mainly into two botanical distinctions — sativa and indica (or “hybrids”, which are a mix of the two). Sativa strains are said to provide a more energetic, cerebral sensation. Indica strains are said to be more relaxing, the type that you’d want to use at night. Many cannabis patients use this distinction in order to decide which strain to use and when to use it.
But there’s actually no scientific evidence to support the notion that the effects a strain has on the user are linked to botanical indicators like indica and sativa. Nonetheless, it’s impossible to completely discount anecdotal evidence and the lived experiences of cannabis patients who know how particular strains affect them.
Finding the perfect strain can be both enjoyable and difficult. First off, our bodies are unique. Some people love spicy food, others prefer sugary food. Some get hyper on coffee and others can drink it right before bed. Two people sharing the same joint can experience different effects, because their body systems react differently to the same substances.
Secondly, just like our bodies, cannabis strains are unique. Cannabinoids and terpenes interact with each other in a way that science is yet to fully understand. But there are some methods you can follow to find the best strain for you — ideally you’ll use a combination of all three:
Cannabis delivery methods mainly fall into one of three categories: inhalation, ingestion, or topical (dermal) application. Each has its own pros and cons.
Inhalation is the most popular delivery method, largely because it’s convenient, simple, fast-acting, and enjoyable. When cannabis is inhaled, it directly enters the lungs en route to being absorbed into the bloodstream, creating almost instantaneous onset. There is also the fact that smoking in and of itself — be it with a pipe, “bong,” or marijuana cigarette (“joint”), can be a therapeutic, enjoyable exercise.
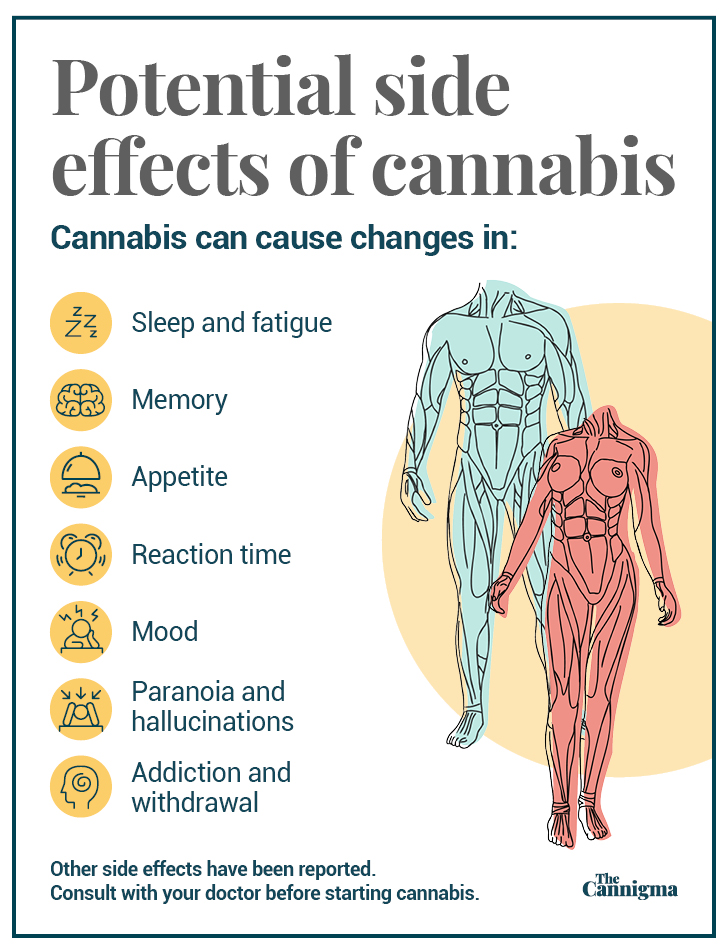
In addition, smoking cannabis can result in many of the same respiratory side effects that are caused by any form of smoking. People with respiratory conditions such as COPD should consider other delivery methods.
Long-term cannabis use can also be habit forming for a small number of users, and like with any substance, it should be used in moderation.
People who have a history of psychosis may be advised to avoid using marijuana due to the risk that THC could exacerbate dissociative or psychotic tendencies.
CBD is also considered quite safe, though it can have some side effects, including changes in weight/appetite, nausea, fatigue, and diarrhea.
In addition to side effects, cannabis can have interactions with a wide range of medications from calcium channel blockers to blood thinners to selective serotonin uptake inhibitors and antidepressants. It can also intensify the effects of depressants like alcohol, barbiturates, and opioids, among others.
Patients who are already on a prescribed medication routine should consult with their physician before starting medical cannabis in order to avoid any adverse drug interactions.
For new patients, discovering the world of medical — or recreational — cannabis can be a bewildering experience at times. That’s partly due to the fact that cannabis is such a complex plant, and the culture and industry surrounding medical and recreational marijuana is so vast. Like with dosing, it’s advisable to start low and slow, and to remember there is an ever-expanding base of research behind the science of cannabis. Furthermore, countless patients and fellow travelers who have been in your shoes before and can provide advice and a helping hand.