

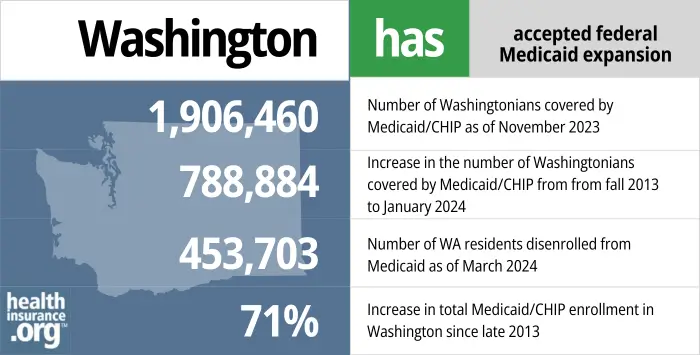
469,000 disenrolled from Medicaid during “unwinding” of pandemic-era rules. Undocumented immigrant adult eligibility began in mid-2024 but enrollment cap was reached within a few days.

Apple Health (Washington’s Medicaid/CHIP) provides health insurance coverage for qualifying children, pregnant women, parents, seniors, and individuals with disabilities. See the Eligibility page on the Washington State Health Care Authority (HCA) website for details. Below is a summary of income limits for non-elderly adults and children, including an additional 5% income disregard that’s used for eligibility determinations: 1
Apple Health is available to children and pregnant women in the allowable income range even if they are undocumented immigrants. And as of July 2024, Apple Health became available to undocumented immigrant adults with eligible incomes. 1 However, there was an enrollment cap of 13,000 for this population, since only a set amount of state funds had been allocated to provide Apple Health to undocumented immigrant adults (federal funding is not available for this). The enrollment cap was reached in just a few days, with the state announcing on July 3 that eligible residents should still submit an application that could “be considered if space opens in the program.” 2
Federal poverty level calculatorof Federal Poverty Level
Apply through HealthCare.gov or by calling 1-800-318-2596 (24 hours a day).
Eligibility: The aged, blind, and disabled. Also, adults with incomes up to 138% of FPL; children with household incomes up to 200% of FPL are eligible for no-premium Medicaid; children with household incomes 200-300% of FPL eligible (with premium); pregnant women with incomes up to 185% of FPL.



Washington was one of five states that utilized a provision in the ACA that allowed for early expansion of Medicaid, before 2014. From 2011 through 2013, Washington used a waiver from CMS to allow for federal funding to cover adults with incomes up to 138% of poverty who were previously enrolled in three state-run programs (Basic Health, Medical Care Services, or Alcohol and Drug Addiction Treatment and Support Act). And the ACA’s full Medicaid expansion took effect in Washington as soon as it became available, in January 2014.
As a gubernatorial candidate in the fall of 2012, Democrat Jay Inslee expressed his support for Medicaid expansion, and he won the election that November. Soon after Inslee took office, he was encouraging lawmakers to move “quickly” to expand Medicaid in line with the ACA’s provisions. Rather than take a formal vote on the issue however, Medicaid expansion was added as a line item to the state budget (with bipartisan approval), and on June 30, 2013, Washington Governor Jay Inslee approved the budget for the upcoming fiscal year.
Washington has also taken steps to ensure access to Medicaid for children and pregnant women, regardless of immigration status, and that’s being expanded to all adults as of mid-2024. 1
 enrollment in Washington since late 2013." width="700" height="355" />
enrollment in Washington since late 2013." width="700" height="355" />

We’ve created this guide to help you understand the Washington health insurance options available to you and your family, and to help you select the coverage that will best fit your needs and budget.


Hoping to improve your smile? Dental insurance may be a smart addition to your health coverage. Our guide explores dental coverage options in Washington.


Use our guide to learn about Medicare, Medicare Advantage, and Medigap coverage available in Washington as well as the state’s Medicare supplement (Medigap) regulations.


Short-term health plans provide temporary health insurance for consumers who may find themselves without comprehensive coverage.

In Washington State, most Medicaid enrollment is managed through the state-run exchange, Washington Healthplanfinder. Unlike private health plans, Medicaid enrollment continues year-round; there is no specific time during the year that you must enroll.
But if you’re 65 or older or have Medicare, use this website to apply for Medicaid and several other social services benefits. You can also request an application by calling 1-877-501-2233. Visit a Department of Social and Health Services (DSHS) Community Services Office to apply in-person for Medicaid for the aged, blind, and disabled; visit a Home and Community Services Office to apply for long-term care benefits.
Many Medicare beneficiaries receive Medicaid financial assistance that can help them with Medicare premiums, lower prescription drug costs, and pay for expenses not covered by Medicare – including long-term care.
Our guide to financial assistance for Medicare enrollees in Washington includes overviews of these programs, including Medicaid long-term care benefits, Extra Help, and eligibility guidelines for assistance.
During the COVID public health emergency, states did not disenroll anyone from Medicaid, even if they no longer met the eligibility criteria. That continuous coverage rule was in place for three years, from March 2020 through March 2023. But in the spring of 2023, states began disenrolling people who were no longer eligible for Medicaid, in a year-long process referred to as the “unwinding” of the pandemic-era continuous coverage rule.
Washington began redetermining eligibility in May 2023, and the first disenrollments were effective as of June. 3 By April 2024, more than 469,000 people had been disenrolled from Apple Health, the majority of whom did not complete their renewal packets 6 (and thus may or may not actually still be eligible for coverage).
People who are no longer eligible for Apple Health can secure new coverage, either through an employer, Medicare, or Washington Healthplanfinder (the state-run exchange/Marketplace). A person’s circumstances will determine which of those coverage options is available to them, but all of them offer a special enrollment period during which a person can transition to the new coverage after losing Apple Health coverage.
People who are eligible for Cascade Care savings can enroll in that coverage at any time (Cascade Care savings is available through Washington Healthplanfinder for people who earn up to 250% of the poverty level and who select a standardized silver or gold plan). For those who aren’t eligible for Cascade Care savings, a special enrollment period was available due to the loss of their Apple Health coverage. Employer-sponsored health plans must have at least a 60-day special enrollment period for people who lose Medicaid. And Medicare has offered a six-month enrollment period for people who lost Medicaid and are now eligible for Medicare.
If a person loses Apple Health but is still eligible (perhaps because they didn’t respond to the renewal packet in time), they have 90 days to complete the renewal and their coverage will be reinstated as if it never ended.
By March 2024, Apple Health enrollment stood at just under 1.9 million people. 3
Enrollment had been higher in 2023, with about 2.3 million people enrolled before the start of the “unwinding” period described above. 5
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org.